This blog breaks down what Integrated Care Systems are and how the changes to data and intelligence will shape the future of population health research.
Download blog in PDF format
- Download infographic - 'Integrated Care Systems: Joining up data and information systems'
What are Integrated Care Systems and what are the population health data and intelligence changes?
What are integrated care systems and what are the implications for population health?
During a person’s life, they will encounter and be supported by a range of local services. These will include the NHS and other care services, but also services associated with factors that influence health such as education, housing, the environment, or employment. By bringing the organisations involved in delivering these services together, moving from competition towards collaboration, the goal is that they will deliver better, fairer health and care for local people. This join up of services is being driven by local partnerships in England called Integrated Care Systems (ICSs). ICSs were formally established on the 1st of July 2022 following the passing of the Health and Care Act (2022) and there are 42 across the country, with six in the East of England.
The structure and functions of ICSs are well summarised in a short explanatory video produced by the King’s Fund. There are two main bodies through which ICSs will operate:
- Integrated Care Board (ICB) – this is a statutory NHS organisation established to take on the functions that were delivered by Clinical Commissioning Groups. Their work includes developing a plan to meet the health needs of the population, managing the NHS budget, and supporting provision of health services in the ICS area.
- Integrated Care Partnership (ICP) – this is a statutory committee jointly formed between the ICB and all local authorities in the area. It has been established to bring together a broad alliance of local partners (membership to be locally agreed but could also include voluntary, community and social enterprise (VCSE) representatives, public representatives, and other partners) to focus on improving the care, health and wellbeing of the local population and develop a cross-system integrated health and care strategy on how to meet local health and wellbeing needs.
ICSs have statutory responsibilities which include working to improve the health and wellbeing of local communities and to tackle inequalities in health. This will involve improving the provision of local services, with the aim of ensuring that local people can get the help and support they need and that services are delivered in a joined-up way that makes the experience as positive as possible.
What does ICS establishment mean for population health data and intelligence and what will change?
Local data and intelligence are central to achieving improved population health and wellbeing. A range of data and research is already used by the individual organisations within an ICS to make decisions about local health and care. This is collectively brought together to produce a local Joint Strategic Needs Assessments (JSNA). JSNAs provide an assessment of the current and future health and care needs of communities and are used to inform local health and well-being strategies and to plan local services.
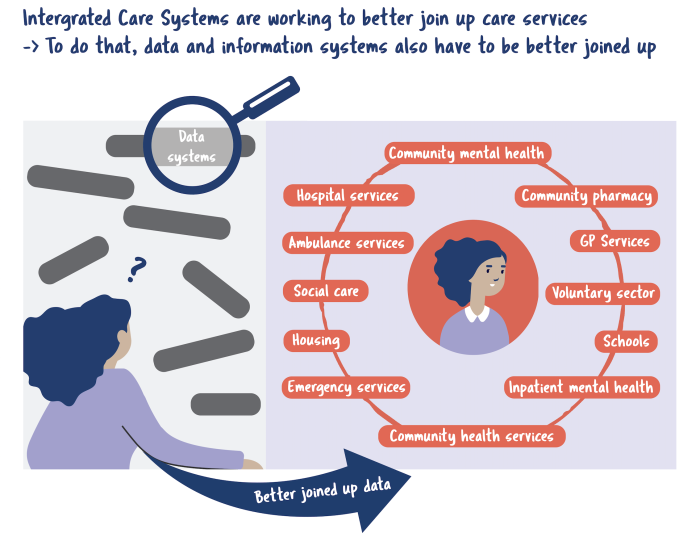
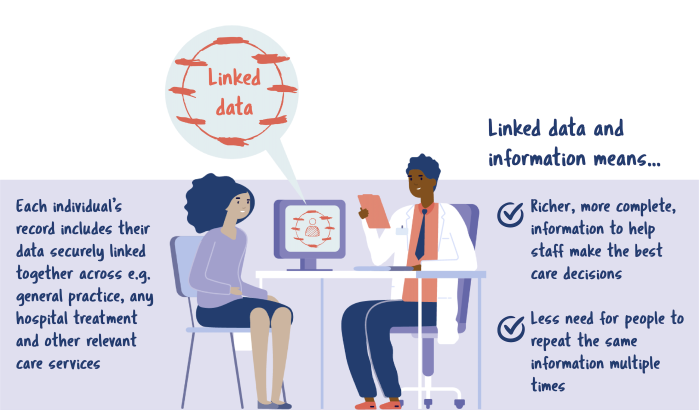
However, the data used are mostly held separately by individual services and their commissioners. This limits the information that can be provided and the questions that can be answered. For example, hospital data is often used to understand local people’s health needs but, while important, hospital visits only provide one part of the picture. If data collected about an individual within different parts of the health and care sector are linked, this will provide a more complete picture of an individual’s current and future health and care needs.
Showing the entirety of an individual’s care will allow a better understanding of which factors have the largest influence on health and care outcomes within the local population. For example, it can help to answer the question of why hospital visits happen and how they could be prevented. This richer range and depth of information will then better inform local strategies and plans for redesigning how care services are delivered to improve health and reduce the risk of poor outcomes and health inequalities.
As ICSs have responsibilities to improve population health, developing and ensuring access to a fully linked individual-level longitudinal dataset across health and care services is an important requirement. This is because such a dataset is needed to underpin the planning and delivery of integrated care. The expectation that ICSs will securely develop a longitudinal dataset linking data from across services has been highlighted in several recent policy documents, with ICS asks outlined below:
- Developing data and digital capability
"Build digital and data expertise and accountability into leadership and governance arrangements, and ensure delivery of the system-wide digital and data strategy”
“[Develop and] ensure use of data and digital solutions to redesign care pathways across organisational boundaries to give patients the right care in the most appropriate setting"
Source: What Good Looks Like framework for data and digital transformation. NHS England. 2021.
- Having accessible longitudinal linked data
"Delivery and development of an ICS-wide intelligence platform with a fully linked, longitudinal data-set (including primary, secondary, mental health, social care and community data) to enable population segmentation, risk stratification and population health management"
What Good Looks Like framework for data and digital transformation. NHS England. 2021.
- Developing intelligence and analytical functions
"Cultivate a cross-system intelligence function to support operational and strategic conversations, as well as building platforms to enable better clinical decisions. This will require ICSs to have linked data, accessible by a shared analytical resource that can work on cross-system priorities"
Integrated Care Systems: design framework. NHS England. 2021.
- Use of linked data to improve population health outcomes
"ICSs use data to design and deliver improvements to population health and wellbeing, making best use of collective resources. Insights from data are used to improve outcomes and address health inequalities"
What Good Looks Like framework for data and digital transformation. NHS England. 2021.
"Using data and analytics to redesign care pathways and measure outcomes with a focus on improving access and health equity for underserved communities"
2022/23 priorities and operational planning guidance. NHS England. 2022.
What do these changes mean for individuals, health and care staff, populations, and researchers?
For individuals: The establishment and availability of fully linked longitudinal data sets offers richer information about the entirety of an individual’s health and care. It means that health and care staff working in services inside and outside of the NHS are aware of all the relevant information to ensure optimal clinical decision making and how to improve an individual’s care. There will also be less need for an individual to repeatedly provide the same information to different services and health and care staff.
For a local population: Securely bringing together individual care records permits analyses that provide more detailed pictures of a) how health and care services are used, and b) health outcomes for different groups in the local population. The information will be anonymised, and will either be depersonalised (information identifying the individual is removed but it still needs to be handled with care as is still about an individual person) or anonymous (information from many people is combined together and it is not possible to identify someone), Further information on these definitions is available in this link. This will support better tailoring and joining up of local services to meet different health needs.
Using and analysing linked data can help identify common factors increasing the risk of developing poor health (e.g., individuals with multiple health conditions, living in a deprived area and with higher use of hospital care). Services can be reviewed, redesigned and joined up to provide a greater focus on prevention of ill health, tailored for those individuals identified with factors increasing their risk, and then ultimately reducing the risk of future poor health.
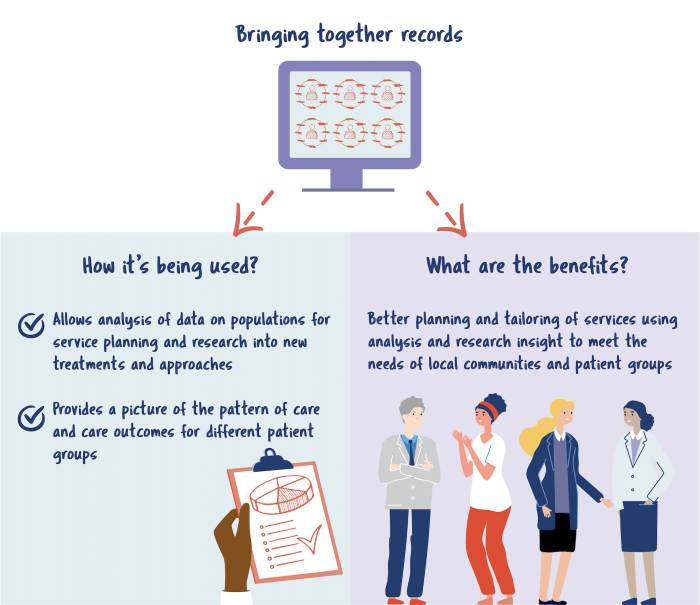
This may involve a need for additional support in a different setting to where the individual presents with a health complaint. This is described in a project carried out in Bristol, North Somerset and South Gloucestershire ICS. Linked data was analysed to identify a group of people with a combination of factors that could put them at a higher risk of developing heart failure. To try to reduce that risk, local support can be agreed to address it and offered to the group through reaching out to them and proactively offering it. As demonstrated in this example, this support could include an annual health check, a medication review, link to peer support, and/or an appointment to discuss personal needs and onward service referral if relevant. These take place in the community and primary care, with a key aim to reduce hospital admissions related to heart failure and the impact of the approach and support offered can be monitored and evaluated.
For researchers: Developments in data and analytics in support of ICS responsibilities offers opportunities to make advances in population health and care research. Key areas of interest building on existing work may include:
Linked data and analytical methods
- Identifying and addressing new research questions that could be answered with new linked datasets
- Ensuring best use of new linked datasets for local services delivery and for research
- Developing and implementing innovative analytical methods
New integrated models of care
- Drawing on insight from emerging linked data and latest research to inform the redesign of existing care models and design of new care models across organisations
- Working with patients and the public to design these new models of care
- Ensuring ethical issues relating to new proactive joined up approaches to care are fully considered such as privacy
- Evaluating these new models of care
Locally relevant research and research-informed local services
- Prioritising shared research questions across the local ICS organisations
- Ensuring the findings from locally relevant research are rapidly disseminated and implemented locally
Conclusion
The goal is that by working together, local services can collectively improve the health of local people and reduce health inequalities. If the research community and their knowledge and skills are part of this endeavour, there are opportunities to advance the areas of interest mentioned above and enhance our knowledge of population health and care issues to the benefit of local services and local people.
End notes:
- For questions relating to the content of this blog, please email ARCoffice@cpft.nhs.uk
- For more information about the Population, Evidence and Data Science research theme, find out more on their webpage.
This blog was written by the PEDS research theme and the infographic was designed by Jo Morton, ARC EoE Comms Lead. The research team would like to thank all who provided valuable comments and input to the development of this blog.