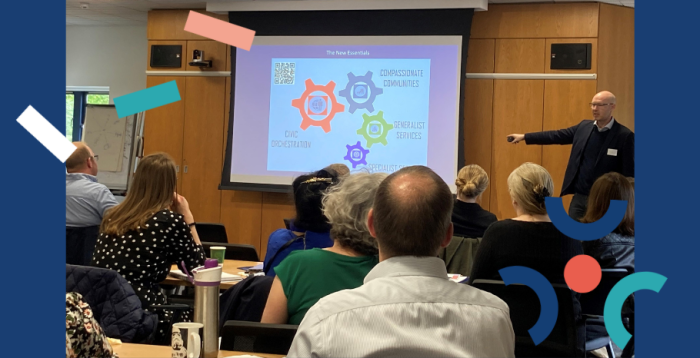
More than 50 people, including cross-ARC researchers, hospice colleagues, GPs, palliative nurses and consultants, and patient and public representatives, joined a Compassionate Communities workshop on Monday 5 June in Cambridge. This event was led by ARC East of England’s Palliative and End-of-Life research theme.
Since 2008, the number of people dying each year in England and Wales has been increasing and this is expected to continue for the next 15 years. There is also an increase in high support needs for longer periods towards the end-of-life. This all amplifies the demand in community care settings to support people approaching death. To address this, compassionate communities aim to empower the affected individual, their carers and families with knowledge on what to do and where to find support in a palliative or end-of-life care context.
Overview of the Compassionate Communities Event
Earlier this month, the Palliative and End-of-Life care research theme led a workshop with the focus of developing more active Compassionate Communities for end-of-life care. The event was attended by 50 cross-ARC researchers, hospice colleagues, health and care professionals, members of the public and patients and community organisations.
Dr Guy Peryer, Research Fellow in our Palliative and End-of-Life care research theme, welcomed everyone to the event and introduced the aims for the day, including encouraging all participants to make a pledge: If something impacts you, what are you going to do about it? There were four talks, followed by a showing of the ‘Care of the Body’ film. Afterwards, Guy facilitated workshop groups to discuss NHS England’s ambition statements.
“There is no shortage of good in our communities, so we need to invite members of the public in the right way to be a compassionate community.”
Dr Guy Peryer, Research Fellow, NIHR ARC East of England
In the first talk, Dr Libby Sallnow, Palliative Medicine Consultation with Central and North West London NHS Foundation Trust, discussed the findings from the Lancet Commission on the Value of Death. Dr Sallnow outlined the Commission, which proposes a new vision for death and dying, with greater community involvement alongside health and social care services and increased bereavement support. The key message from Dr Sallnow’s presentation is that death is integral to life, so making death accessible is key. A well-delivered death should not be denied, and prioritising appropriate care, such as building cohesive networks between healthcare professionals, families, and friends, is important to the wellness of someone’s death.
“Death, dying and grieving affects everyone in the population – it is a population event. Therefore, we need a population response.”
Dr Libby Sallnow, Palliative Medicine Consultation, Central and North West London NHS Foundation Trust
The second presentation was from Norfolk and Norwich University Hospitals NHS Foundation Trusts Palliative Care Consultant, Dr Caroline Barry, on the future directions for Integrated End-of-Life care. Dr Barry reflected on the experiences that she faced during the COVID-19 pandemic and the impact of virtual wards. Dr Barry highlighted the importance of bringing together different groups, from healthcare professionals to charitable and third-sector organisations and provided case studies where this was impactful to an individual’s care. Caroline raised a key statement to the attendees: How would you do palliative care differently? Then do it!
The third talk was led by Jed Jerwood (Principal Art Psychotherapist, Birmingham and Solihull Mental Health NHS Foundation Trust and member of No Barriers Here), who discussed ‘No Barriers Here’, which is an arts-based approach to improve Advanced Care Planning (ACP) to address and understand the needs of people excluded by identity, culture, ethnicity, and race. Jed spoke on behalf of the co-produced group and discussed the process of the arts-based methods, such as exploring who the individual is and what is important to them, who their important people are, and how they want to be remembered. The information gathered from this is then used to educate healthcare professionals. It was highlighted that there are systematic barriers to death and that ethnic minority group’s personal and cultural values are being lost, so these types of discussions are imperative for ACPs. Jed emphasised the need for more open conversations, whether discussing death or what is important to different cultures and ethnicities. Jed ended his presentation by sharing that "a barrier between co-production is feeling it is difficult and it feels hard to do. However, we can take small steps towards co-production and inclusivity."
“We hide death away too much and when conversations need to take place, it is difficult. We have Just-in-Case drugs and I would like to see Just-in-Case conversations.”
Patient and Public Involvement member
The fourth presentation was from Lindsey Crockett (GP, The Peninsula Practice) who explained the interface between services, patients, and end-of-life care volunteers. Lindsey discussed the arc of dying, which is composed of three elements to empower people through the arc of dying and optimise the best death possible: Advanced Care Planning, Resuscitation and Care Wishes. This highlighted the importance for healthcare professionals to ask people ‘what matters to them through all these discussions to enrich death.
Each Community is Prepared to Help
In the afternoon, there was a series of optional focus group discussions designed to share ideas on working with one of NHS England’s ambition statements for palliative and end-of-life care: Each Community is Prepared to Help. These discussions will feed into Developing more active and compassionate communities for Palliative and End-of-Life care, which aligns with NHS England’s ambitions to improve end-of-life care experiences. This workshop specifically aimed to discuss Ambition Six: Each Community is Prepared to Help. To address this, each group explored different key areas, such as expanding community involvement in palliative and end-of-life care in people’s local areas. A number of attendees called for more bereavement services that are community-based and an open dialogue about death.
“A really inspiring event providing an opportunity to make new connections to help promote and share compassionate community’s work. Building confidence to “if it feels uncomfortable, it probably is.”
Karen Hubbert, Compassionate Communities Lead, Keech Hospice Care Luton
Make a pledge to not say 'if' but 'when'
Dr Guy Peryer led the final presentation, where he provided place-based examples of expanding community involvement. For example, the primary school hearts project, which involved the Men’s Shed and the audio play formed at the Suffolk INK Festival. Guy shared the impact of compassionate communities, such as people having the chance to die in their preferred space, thus reducing anxiety, enhancing the interface between acute hospital and communities and successful Rapid Discharge. To enrich people’s experience with death, whether that be the individual’s dying or their families, the change starts with I and Guy called for the attendees to make a pledge, to not say ‘if’ but ‘when’ we will develop more active compassionate communities.
